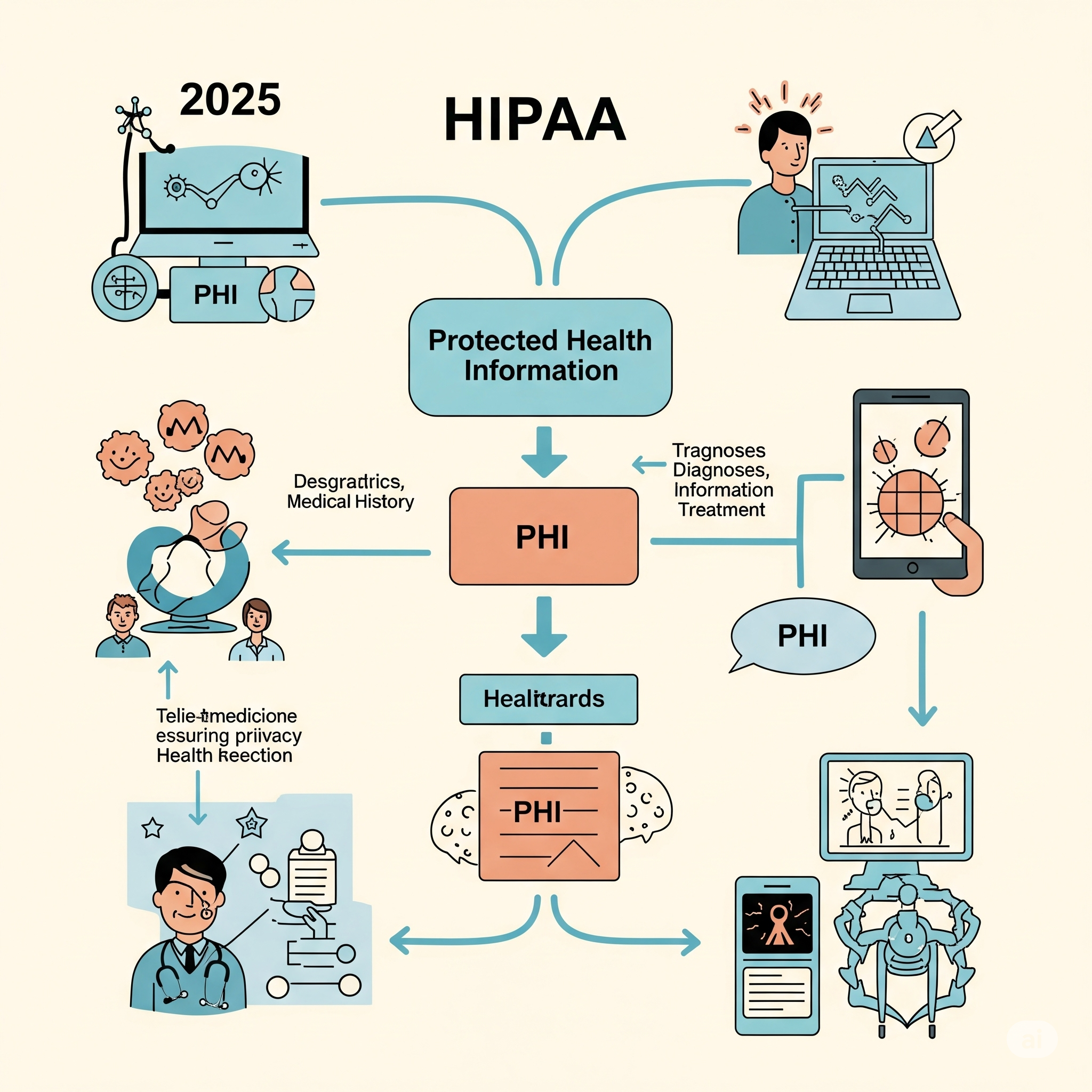
What is HIPAA? Purpose, PHI, & 2025 Relevance
What is the Purpose of HIPAA? A Detailed Overview (Updated for 2025)
The healthcare landscape, increasingly digital and interconnected, relies fundamentally on trust. At the heart of this trust is the rigorous protection of sensitive patient information. The Health Insurance Portability and Accountability Act of 1996 (HIPAA) stands as the cornerstone of health data privacy and security in the United States. While enacted nearly three decades ago, its purpose remains profoundly relevant, continuously adapting to new technologies, evolving cyber threats, and the complexities of modern healthcare delivery in 2025.

HIPAA at a Glance
- Meaning: HIPAA stands for the Health Insurance Portability and Accountability Act of 1996.
- Main Purpose (Concise): Its primary aims were originally to ensure health insurance portability, streamline healthcare administration, and combat fraud. Today, its most prominent purpose is the comprehensive protection of Protected Health Information (PHI), ensuring patient privacy and data security across the healthcare ecosystem.
- Key Components: HIPAA is structured around several critical rules: the Privacy Rule, the Security Rule, the Breach Notification Rule, and the Enforcement Rule.
The Purpose of HIPAA: A Detailed Overview (Updated for 2025)
When HIPAA was signed into law in 1996, its initial objectives addressed pressing concerns within the healthcare system:
- Health Insurance Portability: A core original aim was to improve the portability of health insurance coverage. It sought to limit exclusions for pre-existing conditions and prevent individuals from losing health coverage when changing or losing jobs, thereby empowering individuals to maintain continuous health insurance.
- Administrative Simplification: HIPAA aimed to standardize electronic healthcare transactions (e.g., claims, enrollment, payments). This standardization was intended to reduce the administrative burden, improve efficiency, and lower costs across the healthcare industry by creating a uniform way for entities to exchange information.
- Healthcare Fraud and Abuse Reduction: The Act provided tools and resources for the Department of Health and Human Services (HHS) and law enforcement agencies to combat waste, fraud, and abuse in health insurance and healthcare delivery.
Evolving Purpose and Paramount Importance in 2025
While its original mandates remain active, the focus and perceived purpose of HIPAA have significantly evolved, particularly with the advent of pervasive electronic health records (EHRs), telehealth, and advanced digital health technologies. In 2025, HIPAA's purpose is overwhelmingly centered on:
- Paramount Data Privacy and Security: This is arguably the most critical purpose today. HIPAA establishes national standards for the protection of individually identifiable health information. It dictates who can access PHI, how it can be used and disclosed, and the necessary safeguards to protect its confidentiality, integrity, and availability, especially in the face of sophisticated cyber threats.
- Building and Maintaining Patient Trust: By setting strict rules for data handling, HIPAA fosters essential trust between patients and healthcare providers. Patients are more likely to share sensitive information openly when confident it will be protected, leading to better diagnoses and outcomes.
- Mitigating Cyber Threats: The Security Rule, in particular, acts as a critical framework for cybersecurity in healthcare. It mandates administrative, physical, and technical safeguards to protect electronic PHI (ePHI) from malicious attacks, unauthorized access, and accidental disclosures, a vital function given the high value of healthcare data to cybercriminals.
- Enabling Secure Digital Health Innovation: As healthcare embraces AI, machine learning, and advanced telehealth platforms, HIPAA provides the regulatory guardrails necessary for these innovations to proceed securely and ethically, ensuring patient data remains protected even as technology advances.

Key Components of HIPAA and Their Purpose
HIPAA is enforced through several interconnected rules that define its operational scope:
- The Privacy Rule: Sets national standards for the protection of individually identifiable health information (PHI). It governs the use and disclosure of PHI by Covered Entities (health plans, healthcare clearinghouses, and healthcare providers) and their Business Associates. It also grants patients significant rights over their health information, including the right to access, amend, and receive an accounting of disclosures.
- The Security Rule: Specifically addresses electronic Protected Health Information (ePHI). It mandates administrative, physical, and technical safeguards that Covered Entities and Business Associates must implement to ensure the confidentiality, integrity, and availability of ePHI. Examples include access controls, encryption, audit controls, and physical security measures.
- The Breach Notification Rule: Requires Covered Entities and Business Associates to notify affected individuals, the Secretary of HHS, and, in some cases, the media, following a breach of unsecured PHI. This rule ensures transparency and accountability in the event of a data compromise.
- The Enforcement Rule: Establishes the framework for enforcing HIPAA violations, including procedures for investigations and the imposition of civil monetary penalties (CMPs) and, in certain cases, criminal penalties.
_1750846109.png)
What is Considered PHI under HIPAA?
Protected Health Information (PHI) is the core data element that HIPAA seeks to protect. It is defined as:
Individually identifiable health information created, received, maintained, or transmitted by a Covered Entity or Business Associate, relating to:
- The past, present, or future physical or mental health or condition of an individual;
- The provision of health care to an individual; or
- The past, present, or future payment for the provision of health care to an individual.
Crucially, for information to be considered PHI, it must be individually identifiable. This means there is a reasonable basis to believe the information can be used to identify the individual.
HIPAA PHI: List of 18 Identifiers
Any health information, if combined with one or more of these 18 identifiers, becomes Protected Health Information (PHI) and falls under HIPAA's protections, unless it has been properly de-identified according to HIPAA standards:
- Names
- All geographic subdivisions smaller than a state (e.g., street address, city, county, precinct, ZIP code)
- All elements of dates (except year) directly related to an individual (e.g., birth date, admission date, discharge date, date of death); and all ages over 89 and all elements of dates (including year) indicative of such age, except that such ages and elements may be aggregated into a single category of age 90 or older
- Telephone numbers
- Fax numbers
- Email addresses
- Social Security numbers
- Medical record numbers
- Health plan beneficiary numbers
- Account numbers
- Certificate/license numbers
- Vehicle identifiers and serial numbers, including license plate numbers
- Device identifiers and serial numbers
- Web Universal Resource Locators (URLs)
- Internet Protocol (IP) address numbers
- Biometric identifiers (including finger and voice prints)
- Full face photographic images and any comparable images
- Any other unique identifying number, characteristic,1 or code
Risk Cognizance and HIPAA Compliance
Navigating the complexities of HIPAA in 2025, especially with evolving cyber threats and digital health innovations, requires robust tools. Risk Cognizance provides comprehensive solutions to empower healthcare organizations and their business associates in managing HIPAA compliance effectively:
- Regulatory Compliance Management Software: Centralizes HIPAA requirements, maps them to internal controls, and tracks adherence.
- IT & Cyber Compliance Management Software: Directly supports the Security Rule by managing technical safeguards, security assessments, and cybersecurity policy adherence.
- Policy Management Software: Streamlines the creation, distribution, and attestation of HIPAA-mandated privacy and security policies.
- Case and Incident Management Software: Facilitates efficient management of potential breaches, supporting the Breach Notification Rule's requirements for tracking, investigation, and reporting.
- Integrated Connected GRC Software: Offers a holistic view of HIPAA compliance within your broader Governance, Risk, and Compliance framework, ensuring seamless integration of privacy, security, and operational controls.
_1750846238.jpeg)
Safeguarding Health Information in the Digital Age
HIPAA, initially conceived to address specific healthcare challenges of the late 20th century, has transformed into a foundational pillar for safeguarding sensitive health information in the 21st century. Its enduring purpose is to protect patient privacy, ensure data security, and foster trust in a rapidly evolving digital healthcare ecosystem. For all entities involved in healthcare, understanding and diligently adhering to HIPAA's requirements is not just a legal obligation but a critical commitment to ethical practice and resilient data protection in 2025 and beyond.


